Why after 40 years’ experience as a practising physician, NHS consultant Prof John Wyatt believes we would make a grave mistake if assisted dying became law
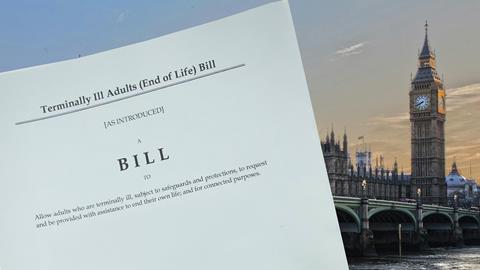
My personal view, after 40 years as a practising physician, NHS consultant and specialist in medical ethics, is that the recently passed Leadbeater Bill adopts the incorrect approach towards providing dignity at the end of life for individuals and their families.
The Leadbeater Bill has fundamentally altered the societal relationship with the medical profession by permitting doctors to assist a terminally ill adult in ending their life through self-administration of lethal substances. For the first time, we now recognise assisting a suicide as exempt from prosecution. Although ‘assisted dying’ may seem positive and compassionate, it signifies a significant shift in the role of doctors from healers to participants in ending patients’ lives.
We all seek compassionate treatment at life’s conclusion. Some supporters perceived the bill as a compassionate response to suffering—despite suffering not being a criterion for eligibility, unlike in other jurisdictions. This ‘choice’ for assisted suicide is restricted to those with less than six months to live, sparking debate about extending it to others suffering from chronic or mental health conditions.
Despite public support, most palliative care doctors oppose this change in law. The bill was debated amidst policies aimed at reducing suicides, defending rights of those with disabilities, and caring for an ageing population with chronic needs worried about becoming a burden on their families and the NHS/social care system. With the Bill’s enactment, assisted suicide might become a regular ‘treatment option’ within the NHS. Our decisions being influenced by our environment means subtle pressures cannot be legislated away.
Practical concerns about the bill’s enactment include challenges in determining prognosis, usage of drugs not licensed or tested for this purpose, potential complications of ingesting lethal substances, impacts on the medical profession, risks of abuse by relatives, and potential for broadening the bill’s application.
Experience from other jurisdictions demonstrates ‘safeguards’ evolving into ”barriers to access”, with criteria expansion beyond terminal illness through court cases. In Canada, laws expanded within five years to include individuals with non-terminal conditions and are due to be extended again to people with mental illness shortly—some choosing death due to inadequate social care.
While some argue palliative care can’t assist all cases, this overlooks its effectiveness in addressing multifaceted end-of-life suffering. The UK leads internationally in palliative care, yet it remains underfunded, relying heavily on fundraising.
Addressing end-of-life suffering should prioritise ensuring all UK terminally ill patients have access to high-quality palliative care before contemplating legalising medically assisted suicide. Addressing this funding crisis and prioritising excellent care must be our main objective.
The report can be found here: www.johnwyatt.com/leadbeaterbill
Dr John Wyatt (www.johnwyatt.com) is a consultant neonatologist and academic researcher who presents Premier Unbeliecable’s ethics show Matters of Life and Death